Health insurance shoppers may wind up with more options to choose from but less help buying a policy under a new Republican proposal to replace the Affordable Care Act.
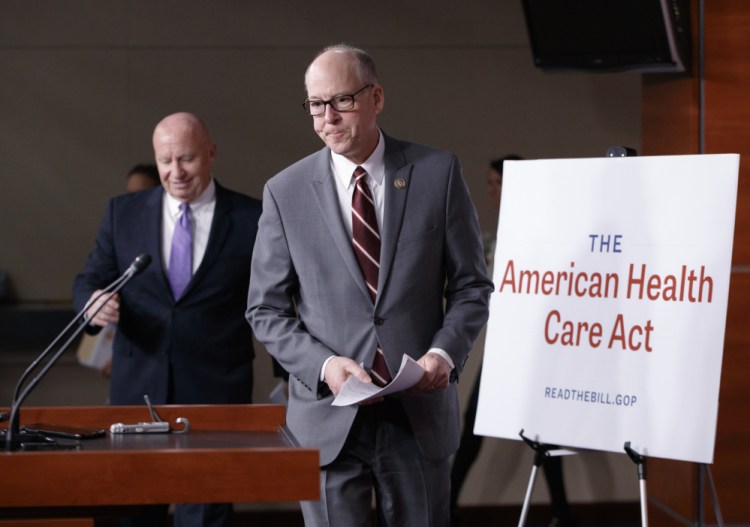
A plan unveiled Monday in the House of Representatives shifts more responsibility for finding affordable coverage to the individual, and away from the government.
Whether the plan becomes law is far from a sure thing – it immediately drew criticism across the political spectrum, and it could change or fail as it makes its way through Congress.
“This is just a first step in what is likely going to be an intense and noisy process,” Stifel health insurance analyst Thomas Carroll said in a research note.
And neither the government’s current plan nor the plan offered by Republicans seems capable of addressing the larger problem, the rising cost of health care that is translating into higher insurance rates, experts say.
“No politician can save you from that,” said Dan Mendelson, CEO of the consulting firm Avalere Health.
But the draft offers the first look at how Republicans want to change the government’s role in delivering health care. Here’s a look at the possible impact:
WILL I PAY MORE FOR INSURANCE?
You might, because you could receive less help from the government.
The Affordable Care Act provides tax credits based on how much money you make to help take the sting out of paying for insurance. The new proposal provides tax credits that are based mainly on your age. These may offer less support for people with low incomes than the current system.
On the other hand, because the new proposal allows for a broader range of insurance plans, it could mean that people may have a better chance of finding a plan they can afford.
WHO WILL THIS HELP OR HURT THE MOST?
Younger, healthier people may have cheaper coverage options, but costs could climb for older patients with chronic conditions and people with low incomes.
The ACA provided subsidies that helped many people with chronic conditions pay out-of-pocket expenses like deductibles, the amount a person has to pay toward care before most insurance coverage starts. Those subsidies could be eliminated under the Republican plan. There’s an option for states to provide such subsidies, but it’s not yet clear how those would work.
And lower-income people may struggle to pay their premiums, the amount due each month for care, because they would get less help from the government.
For example, under the Republican plan, a 41-year-old customer of the insurer Molina Healthcare who earns $20,000 would receive a $3,000 tax credit toward a $4,300 annual premium for one of the company’s plans. That would leave the customer with a bill of $1,300 if there were no cheaper plan available. Under the current system, the government would cover nearly the entire cost of that plan.
WILL THERE BE MORE PLANS TO CHOOSE FROM?
The Republican proposal loosens restrictions on the coverage insurers can offer. That could mean a wider variety of plans, including options with lower prices.
But customers would need to read closely: Plans may come with high out-of-pocket costs like deductibles or narrow networks that exclude the family doctor. The plan may also have less robust coverage of things like mental health care. Those particulars remain far from settled and will probably vary depending on state requirements.
WHAT’S THE PENALTY IF I DON’T SIGN UP?
The Republican plan ends the fines that people have to pay under the ACA if they don’t buy coverage, the so-called individual mandate. But there’s a catch. If people let their insurance lapse for 63 days in the year before they sign up for coverage, insurers could charge these customers 30 percent more for coverage.
WILL MORE INSURERS PARTICIPATE?
That depends on whether lawmakers can fix the insurance exchanges that are leading to large losses for some insurers.
The Republican plan does give insurers something high on their wish list: the chance to offer a wider variety of plans, which might attract younger and healthier customers.
But insurers also are worried that removing the mandate means people will only buy coverage when they are sick, and that makes it very hard for insurers to make money. J. Mario Molina, CEO of Molina Healthcare, said he doesn’t think the 30 percent surcharge is enough of a penalty to entice healthy people to buy insurance.
“I don’t think there’s anything in the bill that makes the market more attractive (for insurers),” Molina said.
AP reporter Ricardo Alonso-Zaldivar contributed to this report from Washington, D.C.
Send questions/comments to the editors.



Comments are no longer available on this story